Periodontitis: Symptoms, Causes, and How It Is Treated
16 September 2020 | Updated: 9 January 2026

Periodontitis, commonly referred to as advanced gum disease, is a serious oral health condition that affects the gums and the bone supporting the teeth. It often develops quietly, with minimal pain in the early stages, which is why many people are unaware they have it until noticeable damage has already occurred.
Left untreated, periodontitis can lead to gum recession, bone loss, loose teeth, and eventually tooth loss. It is also increasingly linked to broader health concerns, including heart disease, stroke, and diabetes. The good news is that periodontitis is largely preventable and, when detected early, very manageable.
In this article, we explain what periodontitis is, how to recognise the symptoms, what causes it, and which treatment options are available.
What Is Periodontitis?
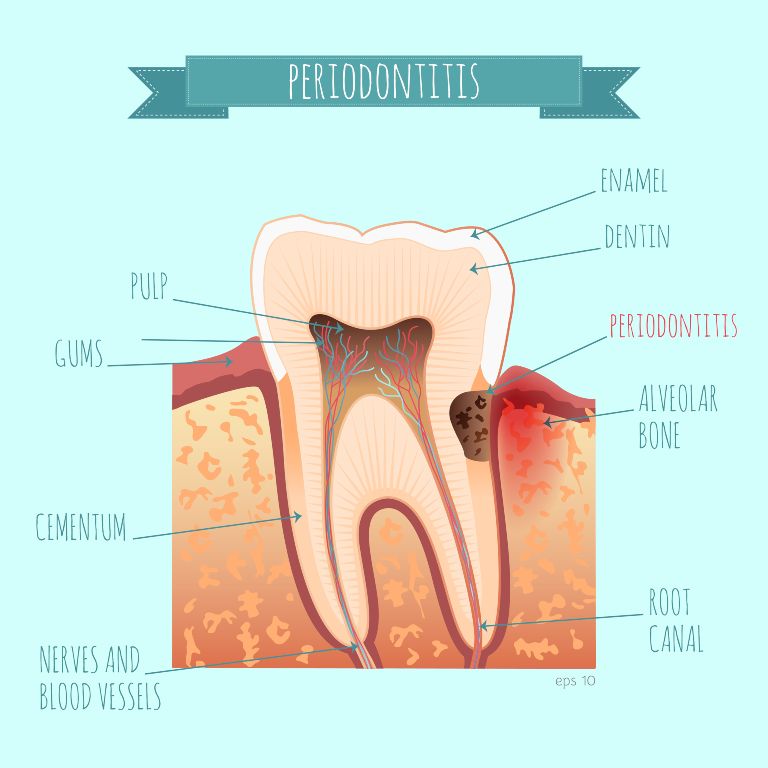
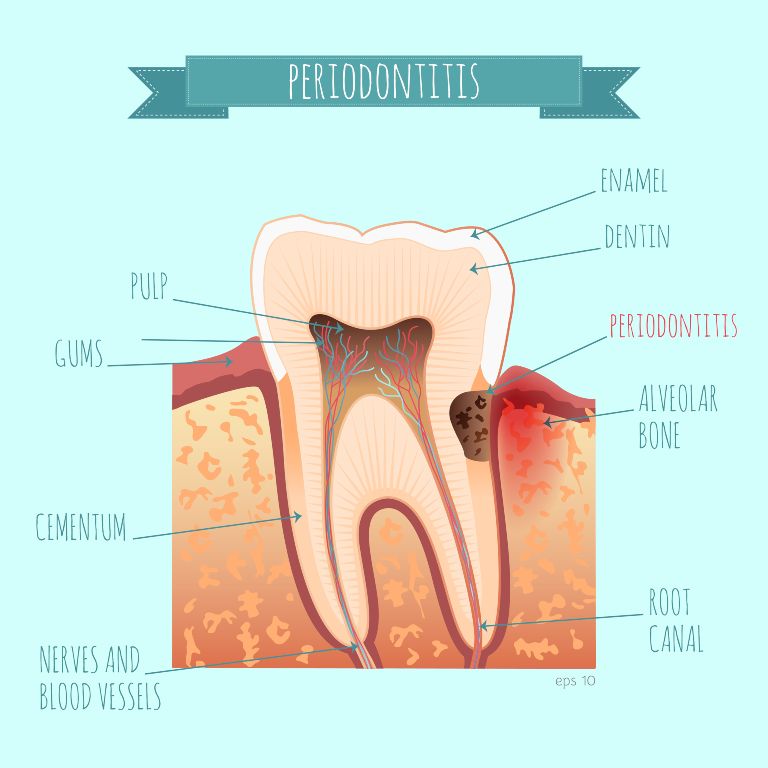
Periodontitis is a chronic inflammatory condition caused by harmful bacteria accumulating around the teeth and beneath the gum line. These bacteria trigger an immune response that leads to inflammation and gradual destruction of gum tissue and the underlying alveolar bone.
The term comes from Greek and means “inflammation around the tooth,” which accurately describes the condition. As plaque and bacteria build up, toxins are released, pockets form between the gums and teeth, and the supporting structures begin to break down.
Without professional treatment, this process continues progressively and can result in permanent damage.
Symptoms of Periodontitis
One of the main challenges with periodontitis is that it often develops gradually and may not cause obvious pain, even as damage progresses. Many patients do not realise there is a problem until significant changes have already occurred.
Common symptoms of periodontitis include:
-
Red, swollen, or tender gums that may feel sore to the touch
-
Gums that bleed easily during brushing, flossing, or eating
-
Persistent bad breath or a constant unpleasant taste that does not improve with cleaning
-
Receding gums, making teeth appear longer than usual
-
Deep pockets forming between the gums and teeth where bacteria can collect
-
Teeth that feel loose, shift position, or begin to separate
-
Changes in how teeth come together when biting or chewing
-
Discomfort or difficulty wearing partial dentures
In some cases, periodontitis may affect only certain areas of the mouth, such as the molars, which makes it easy to overlook without a professional examination. Because symptoms can be subtle or painless in the early stages, regular dental check-ups play an essential role in early detection and effective treatment.
What Causes Periodontitis?
The primary cause of periodontitis is poor or inconsistent oral hygiene, which allows plaque to accumulate. Plaque is a sticky film made up mainly of bacteria. If it is not removed effectively, it hardens into tartar, which cannot be removed by brushing alone.
The disease typically progresses as follows:
-
Plaque forms – when bacteria mix with sugars and starches from food.
-
Tartar develops – if plaque is left undisturbed, trapping bacteria below the gum line.
-
Gingivitis occurs – causing inflammation and bleeding gums.
-
Periodontitis develops – when inflammation becomes chronic, leading to deep gum pockets, bone loss, and tooth instability.
Several factors can increase the risk of developing periodontitis, including:
-
Smoking or tobacco use
-
Untreated gingivitis
-
Hormonal changes, such as pregnancy or menopause
-
Genetics
-
Poor nutrition, particularly vitamin C deficiency
-
Diabetes and other systemic conditions
-
Certain medications that cause dry mouth
-
Conditions that weaken the immune system
Gingivitis vs Periodontitis
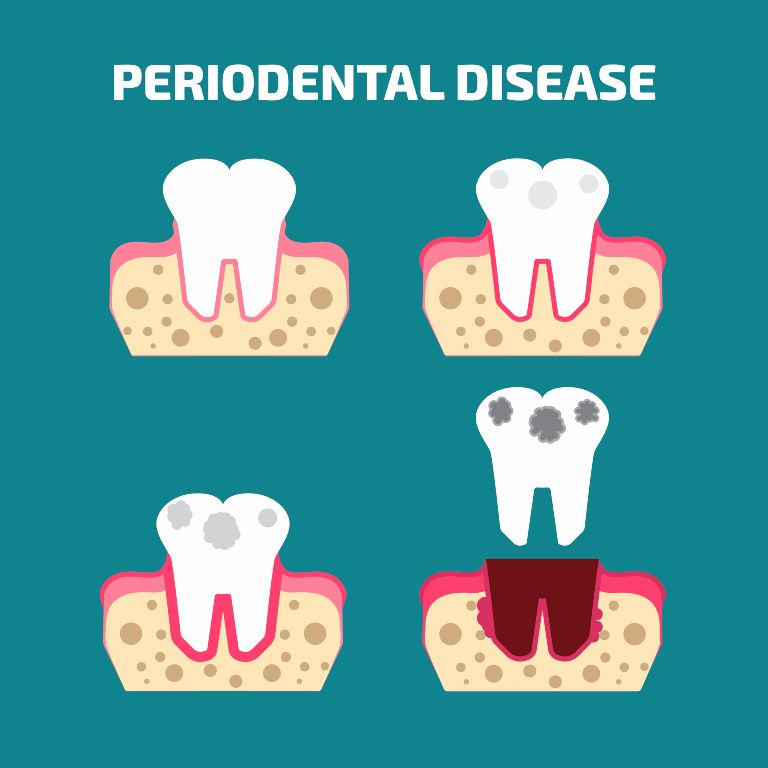
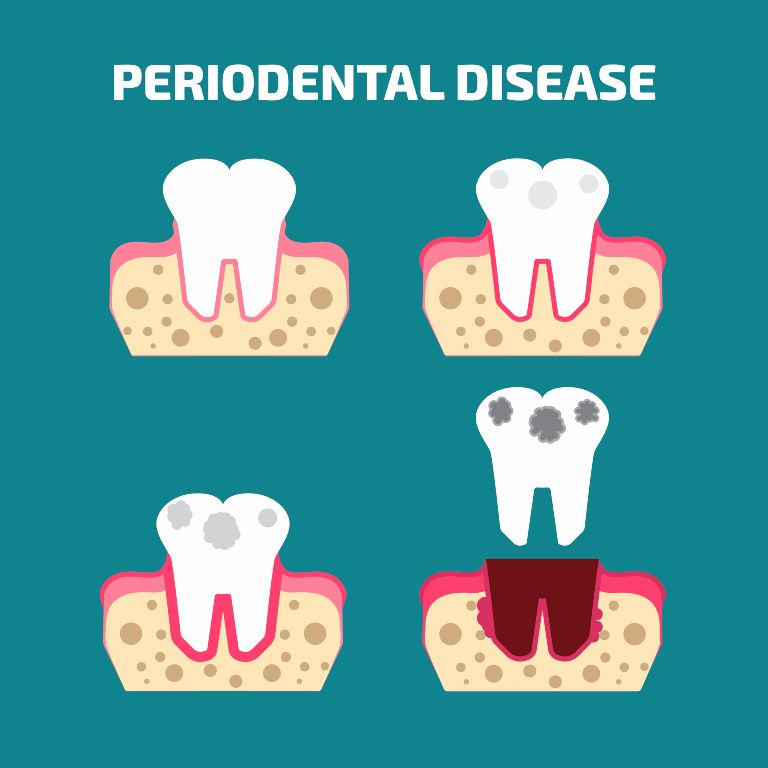
Gingivitis is the earliest and mildest form of gum disease and affects only the gums. At this stage, there is no permanent damage to bone or tissue, and the condition is fully reversible with professional cleaning and good oral hygiene.
Periodontitis develops when gingivitis is left untreated. Once bone and tissue loss occur, the damage cannot be completely reversed, which is why early intervention is critical.
Managing Gingivitis Before It Progresses
Gingivitis is the earliest stage of gum disease and is marked by gum inflammation caused by plaque buildup. Gums may appear red, swollen, or bleed during brushing, but at this stage there is no permanent damage to the bone or supporting tissues. The concern is that untreated gingivitis can progress into periodontitis, leading to more serious and irreversible problems.
The good news is that gingivitis is usually reversible with timely care. Effective management includes:
Professional cleaning, including scaling to remove plaque and tartar below the gumline, is often essential. In some cases, your dentist may recommend targeted treatments such as antimicrobial rinses or gels. Early intervention and consistent oral hygiene are key to preventing gingivitis from progressing further.
Treatment Options for Periodontitis
Treatment depends on how advanced the disease is. Dentists always aim to start with the least invasive approach.
Non-Surgical Treatment
Surgical Treatment
If non-surgical treatment is not sufficient, further options may include:
-
Flap surgery to reduce deep gum pockets and improve cleaning access
-
Bone or tissue grafts to help regenerate lost support
-
Advanced periodontal therapy for severe cases
The most appropriate treatment will depend on the severity and progression of the periodontal disease, but with timely care and close adherence to your dentist’s recommendations, periodontitis treatments are highly effective and can significantly reduce the risk of complications.
Treatment costs in Australia can vary widely depending on severity. Non-surgical treatments are generally more affordable, while surgical procedures may involve higher costs, especially if grafting is required.
Why Early Treatment Matters
Untreated periodontitis does not only threaten your teeth. Ongoing inflammation places stress on the immune system and is associated with increased risks of heart disease, stroke, diabetes complications, and respiratory conditions.
Early treatment can help prevent tooth loss, reduce the need for surgical intervention, lower long-term treatment costs, and support your overall health.
With appropriate care and regular follow-up, periodontal treatment can successfully control the condition and help protect long-term gum and tooth health.
Periodontal Care at MGA Dental Clinic
At MGA Dental clinic, we take gum health seriously. Our team provides thorough periodontal assessments, evidence-based treatments, and long-term maintenance plans to help protect your teeth and overall wellbeing.
If you have symptoms of gum disease or have been diagnosed with periodontitis, contact the MGA Dental clinic in Brisbane or the Gold Coast to book a consultation. Getting treatment early helps protect both your smile and your long-term oral health, while reducing the risk of more serious complications.